Malaria is a constant problem in most parts of the world. Malaria due its causative agent being variable (various species of plasmodium parasites which cause human malaria) and its complicated lifecycle make malaria treatment challenging.
Accurate diagnosis and effective treatment guidelines are crucial in the fight against malaria.
Diagnosis
Diagnosis can be based on the signs and symptoms presented by a patient or on the results of the diagnostic tests.
Signs and symptoms
- Fever and sweating.
- Chills that shake your whole body.
- Headache
- Muscle and joint pain.
- Fatigue.
- Chest pain, breathing problems and cough.
- Diarrhea, nausea and vomiting.
- In extreme cases: jaundice and anaemia

Diagnostic tests for malaria
A lab test confirms malaria parasite infection using a small sample of a patient’s blood experiencing any symptoms (1),
A blood test indicates; the presence of the parasite in the blood, which type of malaria parasite is causing the symptoms or if the infection is caused by a parasite resistant to certain drugs, (2).
Some commonly used diagnostic tests are;
Blood Smear Microscopy
According to WHO, this method is considered the golden standard for laboratory confirmation of malaria.
It usually involves the examination of a blood sample from a patient in a laboratory under a microscope. (3)
Rapid Diagnostic Tests
Rapid diagnostic tests (RDTs) for malaria offer the potential to enhance the management of malaria infections, particularly in remote areas with limited access to microscopy services. RDTs are easy to use, provide quick results, require minimal training, and enable the diagnosis of malaria at the community level. (4)
Polymerase Chain Reaction (PCR)
Parasite nucleic acids are detected using polymerase chain reaction (PCR). Although this technique may be more sensitive than blood smear microscopy, it is of limited utility for the diagnosis of acutely ill patients in the standard healthcare setting. PCR results are often not available quickly enough to be of value in establishing the diagnosis of malaria infection.
PCR is most useful for confirming the species of malarial parasite after the diagnosis has been established by either smear microscopy or RDT. (5)
Proper diagnosis is essential for effective treatment, patient safety, public health, and quality of life. It ensures patients receive appropriate care promptly, minimizes unnecessary treatments, supports disease surveillance and prevention efforts, enables effective condition management, advances medical research, and ultimately leads to improved quality of life and reduced healthcare costs.
Treatment Of Malaria
Treatment is initiated after diagnosis. Treatment should be guided by the following four main factors:
- Infecting plasmodium species,
- Clinical status of the patient,
- Expected drug susceptibility of the infecting parasite as determined by the geographic area where the infection was acquired, and
- Previous use of antimalarials, including those taken for malaria chemoprophylaxis (medication for the purpose of preventing disease or infection).
Malaria treatment is done using antimalarial drugs (which vary depending of the severity of the disease).
Artemisinin-based combination therapies (ACTs) are the most effective antimalarial medicines available today and the mainstay of recommended treatment for Plasmodium falciparum malaria, the deadliest malaria parasite globally.
ACTs combine two active pharmaceuticals with different mechanisms of action, including derivates of artemisinin (extracted from the plant Artemisia annua) and a partner drug (6) . Some of which are:
• Artemether + Lumefantrine
• Artesunate + Amodiaquine
• Artesunate + Mefloquine
• Dihydroartemisinin + Piperaquine
• Artesunate + Sulfadoxine–Pyrimethamine (SP).
The role of the artemisinin compound is to reduce the number of parasites during the first 3 days of treatment, while the role of the partner drug is to eliminate the remaining parasites. (7)
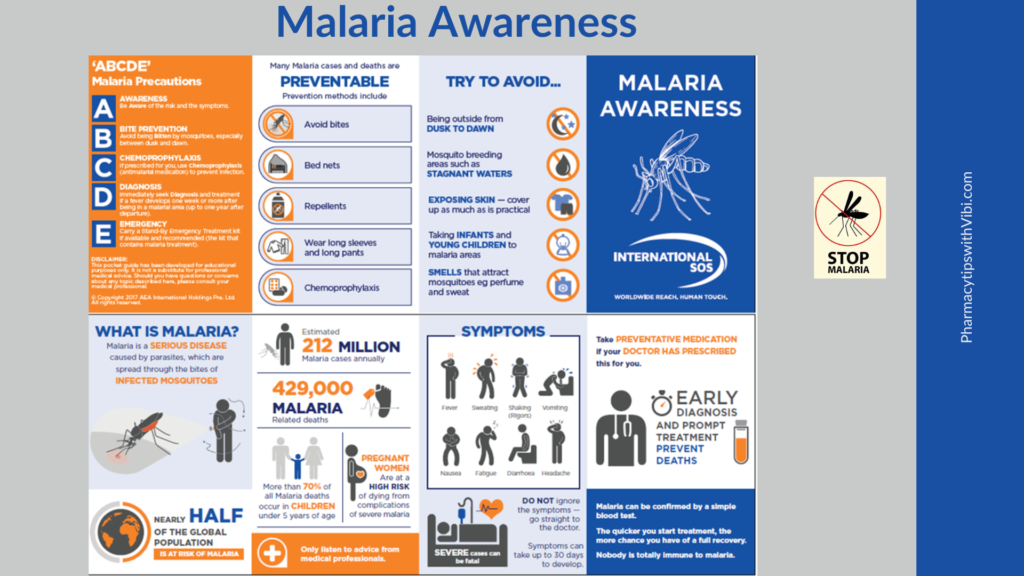
Prevention is better than cure. Malaria can be prevented by;
- Getting Immunised: vaccination and taking of chemoprophylaxis (such as; Primaquine, Chloroquine, hydroxychloroquine, Doxycycline, and Atovaquone-proguanil) by individuals living in or travelling to malaria-endemic areas with dosages varying with respect ot the weight or the type of chemoprophylaxis itself. Always consult with your physician or pharmacist before taking any drug.
- Avoiding Mosquito Bites: Using insecticide-treated bed nets, wearing protective clothing, using mosquito repellents, and spraying houses.
- Destroying Breeding Sites Of Mosquitoes: eliminating standing water, using larvicides in breeding areas, and employing biological control to control mosquito populations and reduce the risk of mosquito-borne diseases.
- Health education: Creating awareness about malaria can help people understand the causes, recognise symptoms, and take better preventive measures.
- Regular Screening For Malaria : for earlier detection.

In conclusion, accurate diagnosis through methods like light microscopy and RDTs (Rapid Diagnostic Tests) and effective treatment of malaria with appropriate antimalarial medications, tailored to the specific parasite and patient’s condition, such as ACTs (Artemisinin-based Combination Therapies ) are crucial in the fight against malaria. Treatment would be easier if patients’ awareness about the disease and drug adherence improves